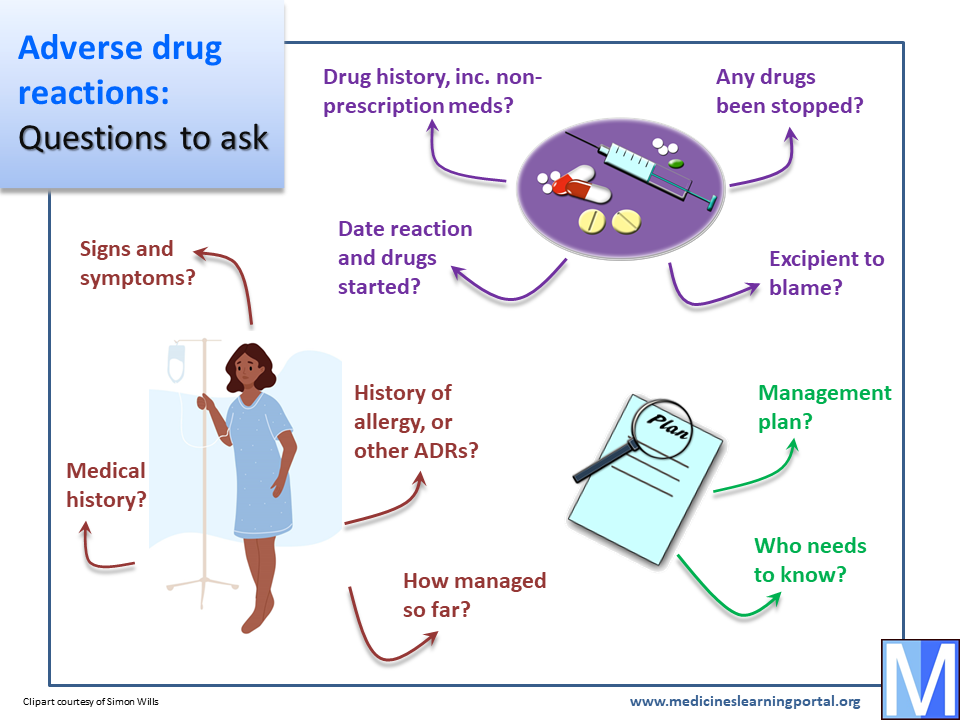
Adverse reactions: Suggested questions
The medicine
- Identify all current and recent medication, including OTC products, complementary medicines and potential substance misuse. It's easy to overlook medicines that have been stopped recently or which have not been prescribed.
- Establish when the suspected reaction began. Which medicines were started beforehand and what were their start dates? The timing of when an ADR presents is often an important clue to which medicine is responsible.
- Has a suspect drug been stopped, and has the ADR improved as a result? Not all ADRs improve quickly after stopping a causative medicine, but any improvement may help to identify the drug to blame.
- Is it possible that an excipient in the medicine is to blame for the ADR rather than the 'active' ingredient? Consider additives as a potential cause if you are struggling to find an obvious cause from an active ingredient. (There is a separate tutorial on this subject.)

The patient
- Ask for details of the suspected reaction including signs, symptoms, and severity. You need to know how the patient has been affected and the results of any relevant investigations. You'll need to clarify vague terms like 'rash' or 'liver impairment'.
- Consider any patient history of ADRs and/or allergies. If the patient has experienced a similar reaction with a related medicine in the past, then this may help to decide which medicine was responsible.
- Ask about any relevant medical history (e.g. concurrent illness) and test results (e.g. blood levels of drug; renal function). Some ADRs may cause deterioration of existing illness; sometimes an existing illness increases the risk of ADRs or makes them more serious (e.g. hyperglycaemia in a patient with diabetes). Importantly, the medical history may also suggest a non-drug cause of the patient's symptoms.
- Ask how the patient has responded to any intervention related to the ADR. Has there been an attempt at e.g. dose reduction or treatment of the ADR?
Going forward
- How is it planned to manage the ADR? What alternative medicine or treatment might be suitable? Is there an existing plan, or can you suggest one? Don't simply identify the likely causative agent: advise on e.g. what can safely be used instead, and how ADR symptoms can be treated. If it's not obvious, you'll need to know what the medicine causing an ADR was being used for, so that you can offer alternatives if it needs to be stopped.
- Who needs to know about this? If your advice is to stop, change or reduce the dose of a medicine, does the patient or their carer understand? If it is due to an allergy has this been properly documented in the patient's notes and have they been told why to avoid the drug in future? Will any prescription changes or monitoring requirements be communicated properly so that the patient's GP knows about them?
The 'questions to ask' from every tutorial on this site have been brought together into a Quick Question Guide that you may want to download for future reference.